Insights on Pressure Injuries in Diverse Skin Tones
October 24, 2024
© 2024 HMP Global. All Rights Reserved.
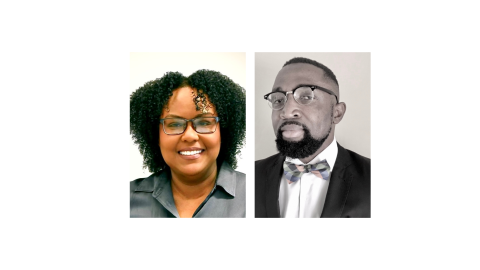
Samuel Nwafor, MD, FACP, FAPWCA:
My name is Dr. Samuel Nwafor, and I'm the medical director for the Wound and Hyperbaric Medicine program at Mountain Vista Medical Center, as well as the Tempe St. Luke’s Hospital, now HonorHealth Hospital, in Tempe, Arizona. I'm also on the board of the National Pressure Injury Advisory Panel, as well as the World Health Organization's working group on wound skin rehabilitation for neglected tropical diseases. I've had faculty appointments previously as adjunct clinical professor of medicine, and I currently teach medical students and residents in a hospital setting and the outpatient setting as well.
Eleonor Pusey-Reid, DNP, RN, MEd:
My name is Eleonor Pusey-Reid. I'm an associate professor here at MGH Institute of Health Profession in Boston, Massachusetts. With over 30 years’ experience, both in teaching and in clinical practice. Most of my clinical practice has been in critical care, adult critical care, and my teaching also has been in the med-surg critical care area and a little bit of research and leadership.
Dr. Nwafor:
So the current staging and identification system does not adequately address the diversity of skin tones and color, particularly in people with dark skin. For instance, a stage one pressure injury is typically defined and described as a nonblanchable area of redness, typically over a bony prominence. While a deep tissue injury on the other hand is described as an area of dark discoloration, again, over a bony prominence. Well, that's much easier to identify in someone with lighter skin, whereas in a person with a darker skin tone, those changes will be more difficult to identify and describe because the skin is already dark. So no wonder we have extensive clinical data that shows that people with darker skin tones have more advanced pressure injuries. They have rates of pressure injuries that are multiple times higher, especially in the advanced stages, compared to people with lighter skin.
One of the most interesting papers on this subject was published by Dr. Joyce Black and some of my colleagues on the National Pressure Injury Advisory Panel showing multiple sets of clinical data that shows that people with darker skin are more likely to be admitted to nursing homes with advanced pressure injuries. And even acute care hospitals, they're more likely to acquire pressure injuries in acute care hospital, and they're more likely to be discharged home with pressure injuries. And also quite interesting is when they get pressure injuries, they're more likely to have them for longer periods of time. So overall, not very good outcomes for people with darker skin.
Dr. Pusey-Reid:
One of the most important factors when we're to identify and prevent pressure injury in darker skin is that early detection is the most, it's a barrier, it’s a big barrier, such as nonblanchable erythema. It doesn't always show up. Similar to what has been taught to clinicians, when we use the description of nonblanching erythema, that usually describes lighter skin manifestation. You might think about redness and nonblanching when we're thinking about description, for example, stage 1, which is not the same in darker skin. In darker skin, you might see subtle hyperpigmentation or darkening around the affected area or at the affected area. This means that clinician needs to use more thorough assessment techniques to be able to catch those early signs, but it may not even be that easy when we're thinking about that. Another issue is that many educational resources that we use primarily describe and normalize light skin tones as the standard so that clinicians are, they're educated to look at manifestations that only describe a certain skin tone or what we say lighter skin tone. And that is why we see a higher incidence of higher, or better said, stage 2, 3, 4 in darker skin tone by the time it's detected. Again, blanching and erythema, they're not often explained or described in our teaching material. My work and my research indicate that when we're looking at textbooks and we are looking at learning materials, we can see that that's the main issue that we are confronting is that the descriptor, it's based on lighter skin tones.
Dr. Nwafor:
So addressing the disparity in assessment and outcomes for people with darker skin and pressure injuries has to come with a multifaceted approach starting with our academic institutions. A study done by Neesha Gunowa and her colleagues out of the UK where they studied multiple academic institutions and looked at their curriculum regarding their training and pressure injuries, that study showed that there was significant deficiency in the curriculum in addressing education, especially to nurses, as it relates to the diversity of skin tones and pressure injuries, particularly with darker skin. So our academic institutions would have to address this in their curriculum, in clinician education. Our health systems, whether it's hospitals, nursing homes, multispecialty practices, outpatient settings, would have to engage in significant clinician education to have their clinicians mindful of this fact and create protocols that will engage clinicians and educate them on the challenges faced in people with darker skins as far as pressure injury go. On an individual level as well. As in medicine, we say, if you're not thinking about it, you are likely to miss it. So on an individual level, the clinician has to be mindful of that In every encounter with a person with dark skin. There are methods of assessment, enhanced assessment skills, that can be taught and easily done and practiced in which you are not just looking for color changes, the use of enhanced physical exam skills, look at and touch the surrounding area, check the temperature, the texture of the skin, because if you're just looking for a color change, it might be absent or difficult to find. They're also other augmented devices that are available these days in looking at pressure injuries as well.
Dr. Pusey-Reid:
So it starts, I think, with education. Clinicians can improve pressure injury identification and prevention in diverse skin tones by using a combination of traditional and advanced methods. Visual inspection alone is not enough for us to detect changes in dark skin, so it's important to use palpation—for example, palpating temperature, firmness, texture—and proper lighting. Lighting is crucial. Natural lighting and angle lighting, or tangential lighting, is one way that we can start to be able to at least recognize that there are some changes that have occurred that require further and advanced assessment that we have taught our clinicians. Using technology is crucial. There are some technologies that are already in the market that we need to normalize and make default at the bedside, make it part of our assessment at the bedside. Devices such as thermography or subepidermal moisture measurement scanners are some of the most recent technology that has been studied, and they're still doing studies, and they have found in our preliminary, in all the studies, that they can detect some early, early changes in all skin tone and especially dark skin tone.
It is also essential that we update how we teach assessment. Educational materials need to reflect a broader range of skin tones, so we can't only focus and normalize lighter skin tones, which leaves out and exclude darker skin and diverse skin tones in our teaching.
From a financial perspective, preventing pressure injury is critical. Hospital acquired pressure injury can cause the healthcare system up to $26.8 billion annually because, to get people to recover and to heal from stage 3 and stage 4, accounts for that bulk of the costs. By investing in prevention and early detection of pressure injury can reduce that burden cost that we are having with pressure injury in the healthcare system. And using not only the descriptors that we currently have, but expanding the descriptor, how you will see manifested in dark skin tone is crucial. And recognizing the use of technology is essential. It should be readily be available at the bedside. This approach will help ensure that we better care for individuals from all different skin tones.
© 2024 HMP Global. All Rights Reserved. Interviews with thought leaders are intended to reflect their individual experiences and observations on a subject matter and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies, nor do they reflect the stance or views of any particular organization, unless specified by the speaker.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.