An Evidence-Based, Sustainable Solution for Wound Management in Low-Resource Settings: Part 2
June 18, 2024
An Evidence-Based, Sustainable Solution for Wound Management in Low-Resource Settings: Part 2
The Available Technology Dressing (ATD) Randomized Controlled Trial
Linda Benskin, PhD, RN, SRN (Ghana), CWCN, CWS, DAPWCA, WOCNF and Richard Benskin
Editor’s Note: This series originally appeared on Today’s Wound Clinic and is adapted with permission. The peer-reviewed article from which this commentary originated is published with Wounds.
Part 1 in the series can be found here.
Knowledge of the basic science of wound healing guided the development of an improvised wound dressing for resource-limited settings in the tropics. The FW dressings used in Japan were modified significantly to accommodate the special needs of patients in a much warmer environment with fewer resources.19,20,41 A Wound Healing Foundation grant helped fund a three-armed,12-week, evaluator-blinded, non-inferiority RCT.42 The study, conducted at the University Hospital of the West Indies in 2021, was registered on ClinicalTrials.gov prior to the first patient visit.41 Sickle cell leg ulcers (SCLUs) became the focus due to their relative homogeneity, relative abundance in Jamaica, and the critical need for a more effective wound dressing solution for these patients.43–46 The added challenge of ischemia helps explain why SCLUs heal 3 to 16 times more slowly than VLUs.45,47,48 SCLUs tend to be recurrent, and are often so painful that opioids are insufficient.45–48
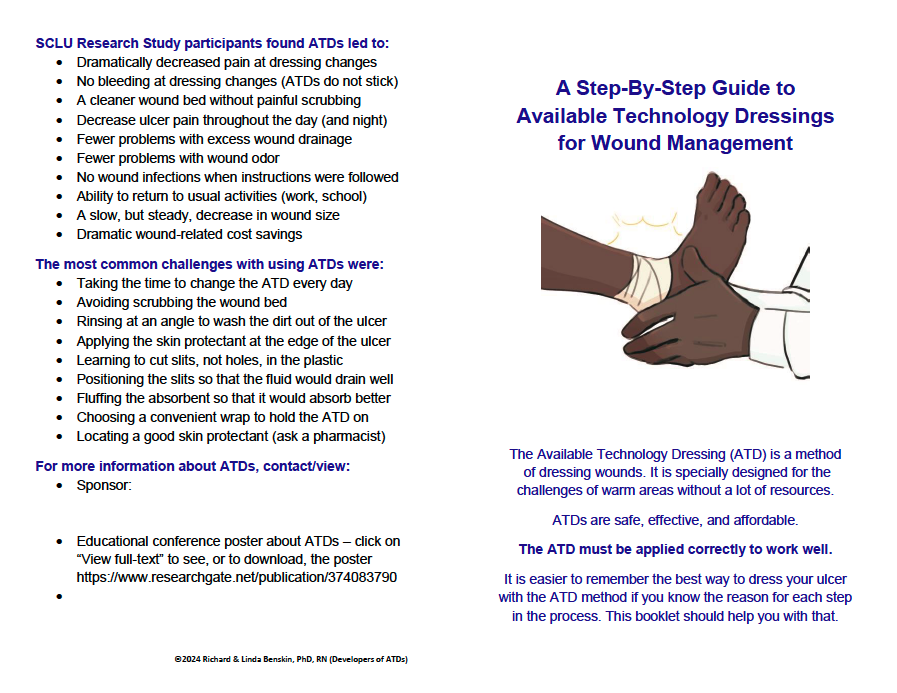
Technology is the application of scientific knowledge for practical purposes.49,50 The improvised dressing was named the Available Technology Dressing (ATD) technique because the study participants demonstrated that accurate implementation is not intuitive to untrained wound patients, and it is critical to its success; careful teaching and demonstration/return demonstration is required.41,51
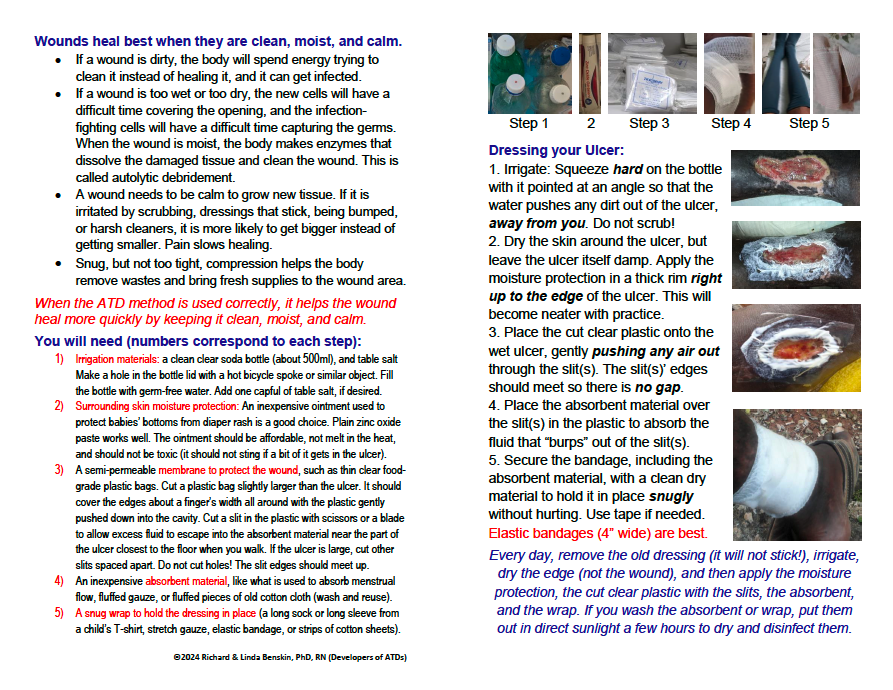
The ATD technique consists of: (1) thorough wound irrigation with strong squeeze on a homemade device (a ~500ml soda bottle with a hole from a hot bicycle spoke in the cap) filled with homemade saline; (2) drying the periwound, then protecting it with a non-toxic moisture barrier (eg, zinc oxide paste); (3) a cut-to-fit piece of food-grade clear plastic bag (a clean semipermeable membrane), with slits to allow excess fluid to escape, gently conformed to the wound bed and the moisture barrier; (4) fluffed clean absorbent material placed over the slits to absorb the excess fluid; (5) all of this held in place (and, when tolerated, compression applied) with a snug wrap.9,41 Daily, the ATD was removed, the wounds were irrigated thoroughly, the periwound was dried, and a new ATD was applied.41,51–53 Exact dressing components can vary based upon availability.
Comparator dressings: Because other wound management methods have not led to superior outcomes, standard of care for SCLUs world-wide is wet-to-dry gauze or dry gauze over an ointment.47,54 However, these dry and adhere to the wound bed, which is not congruent with the goals of lay health practitioners in village settings or modern wound theory.4,55 Therefore, the researchers chose saline-soaked (wet-to-moist) gauze, or WTM, for the usual practice (negative control) arm of the study, fluffing the gauze to help keep it moist.4 The wound was irrigated well, at daily dressing changes.
The Sickle Cell Unit in Mona, Jamaica had trialed many advanced dressings, including honey, Unna boots, FW (used circumferentially, as in Japan), and hydrocolloid dressings, which all failed to produce superior results and/or were not accepted by patients, in part due to the warm climate.41 However, comparing the ATD only to WTM dressings would assure the impending obsolescence of the study results, because saline-soaked gauze is widely regarded as inferior to advanced dressings.56–59
The only advanced wound dressing type with a strong record of success in the tropics is polymeric membrane dressings, or PMDs (PolyMem®, Ferris Mfg. Corp., Ft Worth, TX, USA).14,60 PMDs do not melt, break apart, or adhere to wound-beds in a warm environment, and they are well tolerated in the tropical heat.14,61,62 The continuous cleansing system that is an integral function of PMDs mitigates the problem of increased wound infections in the tropics.14,61 PMDs also control inflammation and decrease pain, two key influencers of healing important for SCLUs.14,60,63 When used on VLUs, even without compression, PMD use led to increased wound closure rates and decreased pain.62,63 PMDs are among the very few advanced wound dressings mentioned favorably in the sickle cell scientific literature.47,64 This made PMDs the logical choice for a positive control.14,61,65–69
Study results: Due to the pandemic, the 40 study participants tended to be older, with large, long-standing SCLUs - all predictors of ulcers increasing, rather than decreasing, in size.41,48 Statistical results were obtained and evaluated by three statisticians to ensure accuracy of interpretation of this small, heterogeneous data set. Participants in all three groups saw improvement in both ulcer closure and quality of life compared with their previous practice. Overall, the ATDs (13 participants) were clinically superior to WTMs (16 participants), and only modestly clinically inferior to PMDs (11 participants) with respect to decreased wound size and pain. ATDs proved to be safe: the only study complications were in the WTM group, with four (25%) patients developing Pseudomonas infections. These resolved quickly when irrigated with 0.5% vinegar, per the study protocol.41
Although Wound Quality of Life and ASCQ-Me Pain scores improved most with PMDs, ASCQ-Me Pain scores improved more in participants using the ATDs than WTMs. Wounds decreased in size much more often with ATDs than with WTMs as well (92% vs 50%). PMDs were by far the least time consuming to use, but ATDs were far less expensive (daily ATD materials costs were half that of WTM costs). Participants in all three groups gave ATDs high marks for acceptability. WTMs, which are commonly used worldwide, were not superior to ATDs by any metric.
Concluding Thoughts
Rigorous surveys confirmed that moist wound management is preferred, even in a tropical environment. However, until now, cost and availability has made it difficult for lay health care providers to provide a moist wound environment. The ATD technique proved safe, effective, affordable, and acceptable on sickle cell leg ulcers in Jamaica, and their use dramatically improved pain scores when compared with WTMs. Although PMDs outperformed ATDs for both pain relief and healing, ATDs were not dramatically inferior, they are far less expensive, and they are far more available. Study participants were able to master the dressing technique quickly, and preferred the ATD technique over other choices. WTMs were inferior to ATDs in every respect. The ATD technique finally provides a sustainable evidence-based solution for wound management in remote and conflict areas of tropical developing countries, and it shows promise for use in other resource-limited environments as well.
This study demonstrated that the proposed ATD concept is sound. All materials (the irrigation device, periwound protectant, primary dressing, absorbent, and wrap) should be chosen for their functional properties and be readily available (which implies affordability) in the setting of the learners. Because the technique must be rigorously followed for the dressing to provide optimal benefits while minimizing risk of complications, the reason for each aspect of the dressing technique must be taught. This will empower the learners with the basic scientific knowledge to know which aspects of each material and which aspects of each step in the technique are critical.
The below figure(s) are used with permission from Linda and Richard Benskin:
Linda Benskin gained extensive wound management experience providing primary care for five years in a remote conflict-prone area of West Africa. She wrote a comprehensive handbook for the self-supporting village health worker training program she developed. The lack of sustainable wound management solutions in this challenging environment drove her to a deeper understanding of the basic principles and physiology underlying wound healing.
Dr. Benskin emphasizes working with the body to promote healing, often with information-dense heavily-referenced articles and presentations. Topics include basic wound healing principles, managing wound infection, pain and inflammation, and the role of vitamin D. She presents at conferences, in classrooms and hospitals, via webinars and podcasts, in church foyers, and under mango trees. Her eager audiences have ranged from experienced surgeons to barely-literate villagers across six continents.
Dr. Benskin works for Ferris Mfg. Corp. and independently with her husband, Richard. The Benskin Research Group developed the Available Technology Dressing technique for resource-limited settings, conducting a grant-supported RCT demonstrating its safety and effectiveness. Linda Benskin was inducted into the inaugural class of WOCN Fellows in 2023.
References
1. Gibbs S. Skin disease and socioeconomic conditions in rural Africa: Tanzania. Int J Dermatol. 1996;35(9):633-639.
2. Mahe A, Hay RJ. Epidemiology and Management of Common Skin Diseases in Children in Developing Countries. World Health Organization; 2005. Accessed February 5, 2015. http://www.who.int/maternal_child_adolescent/documents/fch_cah_05_12/en/
3. Taplin D, Lansdell L, Allen AM, Rodriguez R, Cortes A. Prevalence of streptococcal pyoderma in relation to climate and hygiene. Lancet. 1973;1(7802):501-503.
4. Benskin L 1959. Discovering the Current Wound Management Practices of Rural Africans: A Pilot Study. Dissertation. University of Texas Medical Branch; 2013. Accessed December 29, 2020. https://utmb-ir.tdl.org/handle/2152.3/538
5. Gupta N, Gupta SK, Shukla VK, Singh SP. An Indian community-based epidemiological study of wounds. J Wound Care. 2004;13(8):323-325. doi:10.12968/jowc.2004.13.8.26657
6. Oluwatosin OM. Wound Care Practices and Challenges in Nigeria: Advances in Skin & Wound Care. 2007;20(7):375-378. doi:10.1097/01.ASW.0000280208.98163.1b
7. Ryan TJ. Public health dermatology: regeneration and repair of the skin in the developed transitional and developing world. Int J Dermatol. 2006;45(10):1233-1237. doi:10.1111/j.1365-4632.2006.02671.x
8. Keast DH, ed. Wound and Lymphoedema Management - Focus on Resource-Limited Settings. 2nd ed. World Alliance for Wound and Lymphedema Care; 2020.
9. Benskin LLL. A review of the literature informing affordable, available wound management choices for rural areas of tropical developing countries. Ostomy Wound Manage. 2013;59(10):20-41.
10. Bender DE, Pitkin K. Bridging the gap: The village health worker as the cornerstone of the primary health care model. Social Science & Medicine. 1987;24(6):515-528. doi:10.1016/0277-9536(87)90341-8
11. Benskin LLL. A Concept Development of the Village Health Worker. Nursing Forum. 2012;47(3):173-182. doi:10.1111/j.1744-6198.2012.00270.x
12. Belcher DW, Afoakwa SN, Osei-Tutu E, Wurapa FK, Osei L. Endemic pyoderma in Ghana: a survey in rural villages. Trans R Soc Trop Med Hyg. 1977;71(3):204-209.
13. Benskin L. Incorporating Wound Care in a Christian Village Health Worker Training Program. Poster #2 presented at: 8th Annual American Professional Wound Care Association; April 2, 2009; Philadelphia, PA USA. https://www.researchgate.net/publication/268106196_Incorporating_Wound_…
14. Benskin LL. Polymeric Membrane Dressings for Topical Wound Management of Patients With Infected Wounds in a Challenging Environment: A Protocol With 3 Case Examples. Ostomy Wound Manage. 2016;62(6):42-50.
15. Guenova E, Hoetzenecker W, Kisuze G, et al. Banana Leaves As an Alternative Wound Dressing. Dermatologic Surgery. 2013;39(2):290-297. doi:10.1111/dsu.12067
16. Hoetzenecker W, Guenova E, Moehrle M. Banana leaves: an alternative wound dressing material? Expert Review of Dermatology. 2013;8(5):439-440. doi:10.1586/17469872.2013.835925
17. Toriyabe S, Saito H, Sakurai K. Use of a Food Wrap as a Dressing Material. Advances in Skin and Wound Care. 1999;12(8):405-406.
18. Takahashi J, Yokota O, Fujisawa Y, et al. An evaluation of polyvinylidene film dressing for treatment of pressure ulcers in older people. J Wound Care. 2006;15(10):449-450, 452-454. doi:10.12968/jowc.2006.15.10.26971
19. Takahashi J, Nakae K, Miyagawa M, et al. Plastic wrap as a dressing material to treat stage III/IV pressure ulcers in the inflammatory phase: a randomized controlled trial. Int J Clin Exp Med. 2017;10(3):5586-5594.
20. Bito S, Mizuhara A, Oonishi S, et al. Randomised controlled trial evaluating the efficacy of wrap therapy for wound healing acceleration in patients with NPUAP stage II and III pressure ulcer. BMJ Open. 2012;2(1):e000371. doi:10.1136/bmjopen-2011-000371
21. Takafumi K, Katsunori F, Yayoi N, et al. JSPU Guidelines for the Prevention and Management of Pressure Ulcers (4th Ed.) | Article Information | J-GLOBAL. 日本褥瘡学会誌. 2016;18(4):455-544.
22. Gore MA, Umakumar K, Iyer SP. Polyethylene Surgical Drape Dressing for Split Thickness Skin Graft Donor Areas. In: Gore MA, ed. Skin Grafts. InTech; 2013. doi:10.5772/54195
23. Plastic Bags, Straw and Polystyrene Ban. Jamaica Information Service. Accessed May 31, 2019. https://jis.gov.jm/information/get-the-facts/plastic-bags-straw-and-pol…
24. ruth. Jamaica’s Scandal Bag Ban Explained —. diG Jamaica. Published September 17, 2018. Accessed May 31, 2019. http://digjamaica.com/m/blog/jamaicas-scandal-bag-ban-explained/
25. Parker L. Plastic bag bans are spreading. But are they truly effective? National Geographic. Published April 2019. Accessed May 31, 2019. https://www.nationalgeographic.com/environment/2019/04/plastic-bag-bans…
26. Benskin LLL. The Quest for a Sustainable Wound Management Solution for Rural Areas of Tropical Developing Countries: What We Have Learned So Far. Poster #18 presented at: 29th Annual Nursing & Midwifery Research Conference and 30th Mary J. Seivwright Day; May 30, 2019; Kingston, Jamaica. doi:10.13140/RG.2.2.28503.14247
27. Benskin LLL. A Unique “Story Completion” Research Method For Obtaining Accurate Survey Data. Poster #32 presented at: 29th Annual Nursing & Midwifery Research Conference and 30th Mary J. Seivwright Day; May 30, 2019; Kingston, Jamaica.
28. Asuquo M, Ugare G, Ebughe G, Jibril P. Marjolin’s ulcer: the importance of surgical management of chronic cutaneous ulcers. Int J Dermatol. 2007;46 Suppl 2:29-32. doi:10.1111/j.1365-4632.2007.03382.x
29. Rollnick S, Miller WR, Butler CC. Motivational Interviewing in Health Care: Helping Patients Change Behavior. 1 edition. The Guilford Press; 2007.
30. Langer V, Bhandari PS, Rajagopalan S, Mukherjee MK. Enzymatic debridement of large burn wounds with papain–urea: Is it safe? Med J Armed Forces India. 2013;69(2):144-150. doi:10.1016/j.mjafi.2012.09.001
31. Starley I, Mohammed P, Schneider G, Bickler S. The treatment of paediatric burns using topical papaya. Burns (03054179). 1999;25(7):636-639.
32. Research C for DE and. Questions and Answers about FDA’s Enforcement Action Regarding Unapproved Topical Drug Products Containing Papain. FDA. Published online November 3, 2018. Accessed November 29, 2023. https://www.fda.gov/drugs/unapproved-drugs/questions-and-answers-about-…
33. Benskin L, Bombande P. Complete healing of extensive third-degree burn wound using polymeric membrane dressings. Poster #7 presented at: 7th Annual Australian Wound Management Association Conference 2008; May 7, 2008; Darwin, Australia. https://www.researchgate.net/publication/295741629_Complete_healing_of_…
34. Rosiak E, Madras-Majewska B, Teper D, Łepecka A, Zielińska D. Cluster Analysis Classification of Honey from Two Different Climatic Zones Based on Selected Physicochemical and of Microbiological Parameters. Molecules. 2021;26(8):2361. doi:10.3390/molecules26082361
35. Sunny B, Sulthana L, James A, Sivakumar T. Maggot Infestation: Various Treatment Modalities. The Journal of the American College of Clinical Wound Specialists. 2016;8(1-3):51. doi:10.1016/j.jccw.2018.03.002
36. Whitaker IS, Twine C, Whitaker MJ, Welck M, Brown CS, Shandall A. Larval therapy from antiquity to the present day: mechanisms of action, clinical applications and future potential. Postgrad Med J. 2007;83(980):409-413. doi:10.1136/pgmj.2006.055905
37. Patel BC, Ostwal S, Sanghavi PR, Joshi G, Singh R. Management of Malignant Wound Myiasis with Ivermectin, Albendazole, and Clindamycin (Triple Therapy) in Advanced Head-and-Neck Cancer Patients: A Prospective Observational Study. Indian Journal of Palliative Care. 2018;24(4):459-464. doi:10.4103/IJPC.IJPC_112_18
38. Blechman AB, Wilson BB, Norris R. Myiasis. Medscape Emergency Medicine. Published online February 8, 2019. Accessed November 29, 2023. https://emedicine.medscape.com/article/1491170-overview#a5
39. Deluca G. Wound Myiasis Management: What Works, What Doesn’t. BROWN EMERGENCY MEDICINE. Published October 28, 2022. Accessed November 29, 2023. http://brownemblog.com/blogposts/2022/10/5/wound-myiasis-management-wha…
40. Gliner JA, Morgan GA, Leech NL. Research Methods in Applied Settings: An Integrated Approach to Design and Analysis, 2nd Ed. Routledge/Taylor & Francis Group; 2009:xvii, 469.
41. Benskin L. A Test of the Safety, Effectiveness, and Acceptability of an Improvised Dressing for Sickle Cell Leg Ulcers in a Tropical Climate. clinicaltrials.gov; 2021. Accessed November 29, 2021. https://clinicaltrials.gov/ct2/show/NCT04479618
42. Grants | Wound Healing Foundation. Wound Healing Foundation. Published 2023. Accessed December 2, 2023. https://www.woundhealingfoundation.org/grants/
43. Cumming V, King L, Fraser R, Serjeant G, Reid M. Venous incompetence, poverty and lactate dehydrogenase in Jamaica are important predictors of leg ulceration in sickle cell anaemia. Br J Haematol. 2008;142(1):119-125. doi:10.1111/j.1365-2141.2008.07115.x
44. Serjeant GR. The Natural History of Sickle Cell Disease. Cold Spring Harb Perspect Med. 2013;3(10). doi:10.1101/cshperspect.a011783
45. Singh AP, Minniti CP. Leg Ulceration in Sickle Cell Disease: An Early and Visible Sign of End‐Organ Disease. In: Inusa BPD, ed. Sickle Cell Disease - Pain and Common Chronic Complications. InTech; 2016. doi:10.5772/64234
46. Serjeant GR, Serjeant BE, Mohan JS, Clare A. Leg Ulceration in Sickle Cell Disease: Medieval Medicine in a Modern World. Hematology/Oncology Clinics of North America. 2005;19(5):943-956. doi:10.1016/j.hoc.2005.08.005
47. Minniti CP, Eckman J, Sebastiani P, Steinberg MH, Ballas SK. Leg Ulcers in Sickle Cell Disease. Am J Hematol. 2010;85(10):831-833. doi:10.1002/ajh.21838
48. Flattau A, Gordon H, Vinces G, Ennis WJ, Minniti CP. Use of a National Electronic Health Record Network to Describe Characteristics and Healing Patterns of Sickle Cell Ulcers. Adv Wound Care (New Rochelle). 2018;7(8):276-282. doi:10.1089/wound.2018.0788
49. Britannica.com. Technology. Published October 16, 2023. Accessed December 1, 2023. https://www.britannica.com/technology/technology
50. CODATA, The Committee on Data for Science and Technology. Technology. CODATA, The Committee on Data for Science and Technology. Accessed December 1, 2023. https://codata.org/rdm-terminology/technology/
51. Benskin L. Trial of an Improvised Dressing for Remote and Conflict Areas of Tropical Developing Countries. Presented at: Technology in Wound Care Conference: AAWC 2022; 2022; Salt Lake City, Utah USA. Accessed February 27, 2023. https://rgdoi.net/10.13140/RG.2.2.10887.06565
52. Benskin LL. Trial of an Available Technology Dressing for Resource Limited Settings. Poster #204 presented at: NCCHC Spring 2023; May 1, 2023; New Orleans, LA, USA.
53. Venugopal R, Benskin L, Barton-Gooden A. Trial of an Available Technology Dressing for Resource Limited Settings. e-Poster presented at: Wild On Wounds 2023; September 14, 2023; Hollywood, FL, USA. https://www.researchgate.net/publication/374083790_Trial_of_an_Availabl…
54. Martí-Carvajal AJ, Knight-Madden JM, Martinez-Zapata MJ. Interventions for treating leg ulcers in people with sickle cell disease. Cochrane Database Syst Rev. 2021;2021(1):CD008394. doi:10.1002/14651858.CD008394.pub4
55. Bolton LL. Common Nonsense: Rediscovering Moist Wound Healing | Wound Management & Prevention. Wound Management & Prevention Journal. Published 2012. Accessed May 26, 2019. https://www.o-wm.com/blog/common-nonsense-rediscovering-moist-wound-hea…
56. Flint L. Invited commentary on “Modern wound care for the poor: a randomized clinical trial comparing the vacuum system with conventional saline-soaked gauze dressings” by Perez et al. The American Journal of Surgery. 2010;199(1):21. doi:10.1016/j.amjsurg.2009.01.030
57. Jones AM, San Miguel L. Are modern wound dressings a clinical and cost-effective alternative to the use of gauze? Journal of Wound Care. 2006;15(2):65-69. doi:10.12968/jowc.2006.15.2.26886
58. Sadati L, Froozesh R, Beyrami A, et al. A Comparison of Three Dressing Methods for Pilonidal Sinus Surgery Wound Healing. Adv Skin Wound Care. 2019;32(7):1-5. doi:10.1097/01.ASW.0000558268.59745.d2
59. Yastrub DJ. Relationship between type of treatment and degree of wound healing among institutionalized geriatric patients with stage II pressure ulcers. Care Manag J. 2004;5(4):213-218.
60. Benskin LL. Evidence for Polymeric Membrane Dressings as a Unique Dressing Subcategory, Using Pressure Ulcers as an Example. Adv Wound Care (New Rochelle). 2018;7(12):419-426. doi:10.1089/wound.2018.0822
61. Feliciano I, Castillo R. Blast Injuries Successfully Managed with PolyMeric Membrane Dressing*. Poster presented at: Philippine Wound Care Society (PWCS); October 22, 2014; Manila, Philippines.
62. Benskin L. Deep Ulceration Treated with Polymeric Membrane Dressings Until Complete Wound Closure. Poster #0727 presented at: 3rd Congress of the World Union of Wound Healing Societies; June 4, 2008; Toronto, Ontario Canada.
63. Agathangelou C. How We Resolved the Problem of Poor Compliance with 20 Chronic Ulcers Patients by Using PolyMeric Membrane Dressings. Poster presented at: European Wound Management Association (EWMA); May 15, 2013; Copenhagen, Denmark.
64. Campton-Johnston S, Wilson J, Ramundo JM. Treatment of painful lower extremity ulcers in a patient with sickle cell disease. J Wound Ostomy Continence Nurs. 1999;26(2):98-104.
65. Benskin L. Excellent healing of pediatric wounds using polymeric membrane dressings... 41st Annual Wound, Ostomy and Continence Nurses Annual Conference, St. Louis, Missouri, June 6-10, 2009. Journal of Wound, Ostomy & Continence Nursing. 2009;36(3S):S14-S14.
66. Benskin LL. Dissecting Hand Abcess Wound Treated with Polymeric Membrane Dressings* Until Complete Wound Closure. Poster #31 presented at: 19th Annual Symposium on Advanced Wound Care (SAWC); May 30, 2006; San Antonio, TX.
67. Benskin L. Diabetic foot salvaged, wounds closed in only two months using polymeric membrane cavity filler* and polymeric membrane dressings. Poster presented at: 39th annual meeting of the Wound Ostomy Continence Nurses Society (WOCN); June 10, 2007; Salt Lake City, UT.
68. Benskin L. Extensive tunneling lower leg wounds with exposed tendons closed quickly using various polymeric membrane dressing configurations. Poster #41 presented at: 23rd Annual Clinical Symposium on Advances in Skin & Wound Care; October 26, 2008; Las Vegas, NV USA.
69. Benskin LL. Spreading the Revolutionary Message of Modern Wound Management Principles: Facilitating Change Among Surgeons. Poster # CS16-031 presented at: WOCN Society & CAET Joint Conference; June 4, 2016; Montreal, Canada.
The views and opinions expressed in this content are solely those of the contributor, and do not represent the views of WoundSource, HMP Global, its affiliates, or subsidiary companies.